Varicose Vein Treatments
Varicose Vein Treatments at Madison Medispa
Madison Medispa offers the safest, most comprehensive varicose vein treatments currently available, all done on an outpatient basis with no need for surgery or general anesthesia.
VARICOSE VEIN TREATMENTS
DIAGNOSTICS
Upright Duplex Ultrasound Venous Flow Mapping
If you are found to have varicose veins, the first step in your treatment will be a venous flow mapping. The “map” is an upright (standing) diagnostic Duplex ultrasound. This procedure takes 1.5 – 3.0 hours.
How Does Duplex Ultrasound Venous Flow Mapping Work?
Diagnostic ultrasound is a non-invasive technique which uses sound waves to image inside your body. When used for venous flow mapping, it allows us to see the size and location of all your veins. It also gives us detailed information about how all of your veins are functioning.
The so-called “map” allows us to develop the best plan of care specific to your needs. Since venous reflux is gravity dependent, your venous flow mapping should always be done while you are standing!
What is a Venous Flow Mapping and why should it ALWAYS be done standing?
This diagnostic ultrasound scan will fully evaluate all of the deep and superficial veins in your leg(s). It will determine which veins are broken and which are normal. It will also show us the flow patterns and interconnections that will help determine your best plan of care.
Please note that a standing ultrasound venous flow mapping is the pre-treatment standard of care. It should be done prior to ALL treatments being planned for varicose veins. If you have been scanned while lying down at another facility, you should request the study be repeated while you are standing. The reason this is so crucial is because vein disease is gravity dependent. Therefore, a recumbent scan is much less likely to detect all areas of venous back-flow or “reflux.” It will also falsely lower measurements of reflux time and vein size! This is important for a variety of reasons. Foremost is because insurance uses all of those data points to determine if they will cover your treatment!
VARICOSE VEIN TREATMENTS
Treatment is typically done in 3 stages:
1.) During the first stage, the main varicose trunk is treated.
2.) During the second stage, the branches coming off the main trunk are treated.
3.) Finally, in the third stage, any remaining spider veins are treated.
VARICOSE VEIN TREATMENTS
Stage 1: Treating the main trunk
In the past, this was done with a very large and invasive surgery called “surgical ligation and stripping.”
Stripping has fallen out of favor and is now rarely utilized by physicians who specialize in vein treatment. This is because the results do not justify the pain, expense, and high risk of this surgery.
Instead, most physicians use endovenous thermal ablation to treat any broken trunks.
Endovenous Thermal Ablation
(Laser or Radiofrequency)
What They Treat:
The large varicose trunks like the Great Saphenous Vein, Small Saphenous Vein, Anterior Accessory Saphenous Vein, and some Perforating veins. All of these veins are deep to the surface and rarely if ever visible without the use of ultrasound.
Procedure Time:
Approximately 60-90 minutes.
Typical Recovery Time and Side Effects:
You can be back on your feet, and even back to work immediately following this procedure! A compression stocking is required for one week. Most patients will say it feels like a mild pulled muscle with some tightness and soreness in the treated area.
Results:
We now have 15-year data demonstrating <2% recurrence of a treated vessel.
How Does Thermal Ablation Work?
Thermal ablation has replaced surgical stripping for the treatment of the largest varicose veins. A small laser fiber or radiofrequency catheter is inserted inside the vein under ultrasound-guidance. Energy in the form of heat permanently seals the vein shut as the fiber or catheter is withdrawn. Your body then dissolves the small vein remnant over the next few months.
VARICOSE VEINS TREATMENTS
Stage 2. Treating the branches
Like the treatment for the large trunks, in the past surgical treatments were heavily utilized. Various types of phlebectomy have been widely used. These procedures physically remove the broken or varicose branches to varying degrees.
Unfortunately, most phlebectomy procedures will result in incomplete treatment leaving many broken branches in the leg. This is because they are reliant on the physician being able to visualize the branches during the procedure, rather than using ultrasound.
A better option for most patients is ultrasound-guided foam sclerotherapy. This procedure uses ultrasound to guided a series of injections into ALL the remaining broken branches. This treatment is much less invasive than any surgery, and it will result in a more complete treatment. It will provide the most comprehensive cosmetic and symptomatic improvement available.
Ultrasound-guided foam sclerotherapy
(Including Varithena)
What It Treats:
This procedure is used to treat the branch veins left over after the endovenous laser has sealed the main trunks. It can also be used to treat any form of recurrence, even after a prior procedure such as a vein stripping. Branch veins are typically the large rope-like veins that patients may be able to see on the surface of their skin.
In our opinion, this is the single most important procedure you need to achieve both cosmetic and symptomatic relief of your varicose veins. If your provider does not offer this service, it is extremely likely your treatment will be incomplete, and you will not be totally satisfied with your results!
Procedure Time:
Typically 60-90 minutes.
Typical Recovery Time and Side Effects:
You will be placed in a compression stocking and can be up and walking immediately after treatment. You will be asked to go home and keep your leg elevated for the remainder of the afternoon after your first ultrasound-guided foam sclerotherapy session.
During the first 12 hours, you will typically have some aching and mild discomfort but this is usually resolved by the following morning. You will typically use a compression stocking for 2-4 weeks after the first treatment. The most common side effects are bruising and trapped blood, both of which resolve on their own.
Results:
Injected branches will begin to scar down and slowly resolve over the next 3 months.
How Does Ultrasound-Guided Foam Sclerotherapy Work?
Ultrasound-guided sclerotherapy is performed by injecting a foamed sclerosing solution into the targeted veins under ultrasound guidance.
The sclerosant foam is easily visualized using ultrasound so we can very easily see which veins have been treated and which veins have not. The solution damages the vein wall, and this will result in destruction of the targeted vein. The body will then slowly dissolve the small vein remnant over the next few months.
This treatment allows for the most complete treatment of patients with varicose veins. It will provide you with the best combination of symptomatic and cosmetic improvement currently available.
Ambulatory Micro-Phlebectomy
What It Treats:
This procedure is used only for the treatment of large localized superficial branch veins. Branch veins are typically the large rope-like veins that patients can see on the surface of their skin. We view this procedure primarily as a cosmetic quick-fix. It should only be for one or two branches for a patient with a very limited time frame for treatment.
Procedure Time:
Typically 60-120 minutes.
Typical Recovery Time and Side Effects:
You will be placed in a compression bandage with a stocking over it. You can be up and walking immediately after treatment. Most patients will be asked to go home and keep their leg elevated for the remainder of the afternoon. There can be some very minor bleeding in the treated areas with subsequent bruising. You will typically use a compression stocking for 2-4 weeks after this treatment.
Results:
Local branches will be gone immediately. Small insicions will heal over the next 2-weeks and should not leave a scar.
Some bruising in the treated area is common and should be resolved within 2-weeks.
How Does Ambulatory Micro-Phlebectomy Work?
Ambulatory micro-phlebectomy is performed by making a series of very small incisions in the skin next to the diseased vein under local anesthesia.
The vein is then removed through the incisions. The incisions are so small they typically will not leave a scar.
VARICOSE VEIN TREATMENTS
Stage 3. Treating the spider veins
Some patients will still have some spider veins remaining after they have completed stages 1 and 2. If so, we can easily get rid of them and provide the cosmetic appearance you desire.
Some patients are even surprised to learn that by treating the remaining spider veins, they can even get additional symptomatic relief!
Click here to learn more about spider vein treatment:
“I came to Dr. Erdman’s office on the advice of my daughter who also had treatment here. I have been very satisfied with my care here and I would absolutely recommend them to anybody who is thinking about having their veins treated.”
– V. H.
Frequently Asked Questions About Vein Treatments
What happens at a consultation?
We will ask you to fill out a brief medical history form concerning your general health and your vein problem.
If you are coming in for your leg veins, a screening ultrasound evaluation of both legs will be done to determine what, if any, vein problems are present. Your areas of concern will be examined and all your questions will be answered. We will discuss what it is that you want to accomplish and how best to achieve your goals.
All possible treatment options will be explained to you, not just the treatments that we provide. Should you select a procedure that we do not perform, we will attempt to refer you to a reliable physician experienced in that procedure. Whatever you decide is fine, but we want you to make an educated choice.
Your consult will last about 60 minutes.
Will insurance cover my treatment?
If you are coming in for purely cosmetic purposes, no. If, however, you are having symptoms or other complications related to your vein disease, vein treatment procedures are often reimbursed by insurance and Medicare, and you may be eligible for benefits. This will be determined on a case by case basis, and will depend on your individual insurance policy. We can never guarantee coverage. Whatever the case may be, we will inform you about what you can expect financially PRIOR to beginning your treatment, and our billing specialist will work with you and your insurance provider to expedite this process.
Don't I need these veins? Where does that blood go? What happens to my circulation?
No you don’t need them. You have miles of superficial veins in your leg, and what we will treat is just a small fraction of the total. Moreover, your vein disease did not develop overnight. In most cases, it will have taken years to get to the point at which you begin to consider treatment. Therefore, your body has literally had years to redirect the venous blood flow in your leg into the miles of good veins. When we treat your broken veins, and alleviate the back pressure coming down the leg in the wrong direction, your circulation will improve!
What if I need a coronary artery bypass? Won't the doctor need this vein?
The greater saphenous vein (along the inseam of your leg) is often used for bypass surgery, but only if it is a normal vein, not if it is a varicose vein. There are multiple alternative vessels to use for bypass grafting.
I am on Coumadin or another blood thinner. Can I be treated?
Yes, in most cases. The procedures we perform are so minimally invasive that there is no significant blood loss associated with them. Therefore, most patients will not have to stop their blood thinners around the time of treatment.
Another doctor said my only option was surgical stripping, and that nothing else will work. Is this true?
This is almost always false. Most patients now have multiple successful options available for their treatment, all of which are much less invasive than surgical stripping.
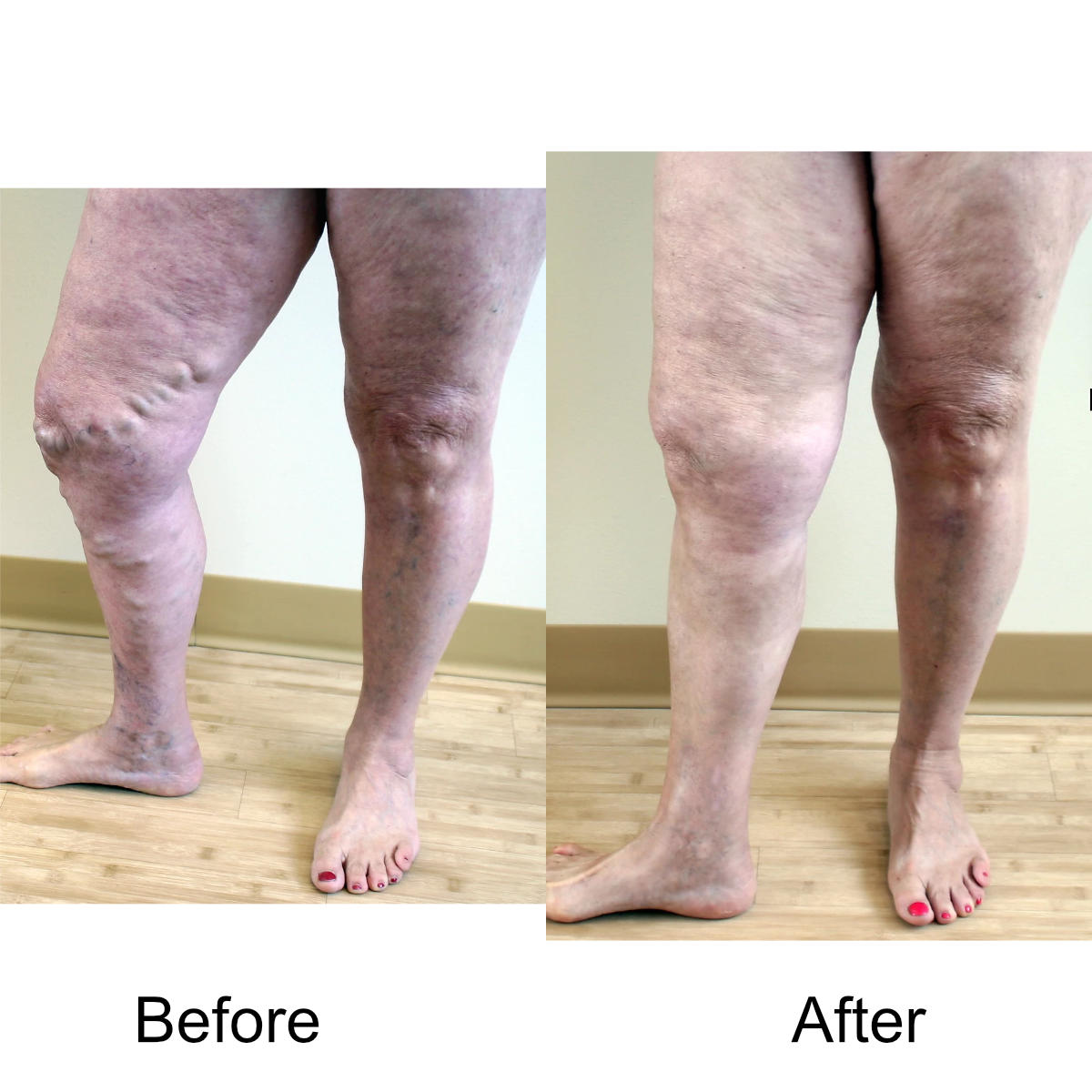
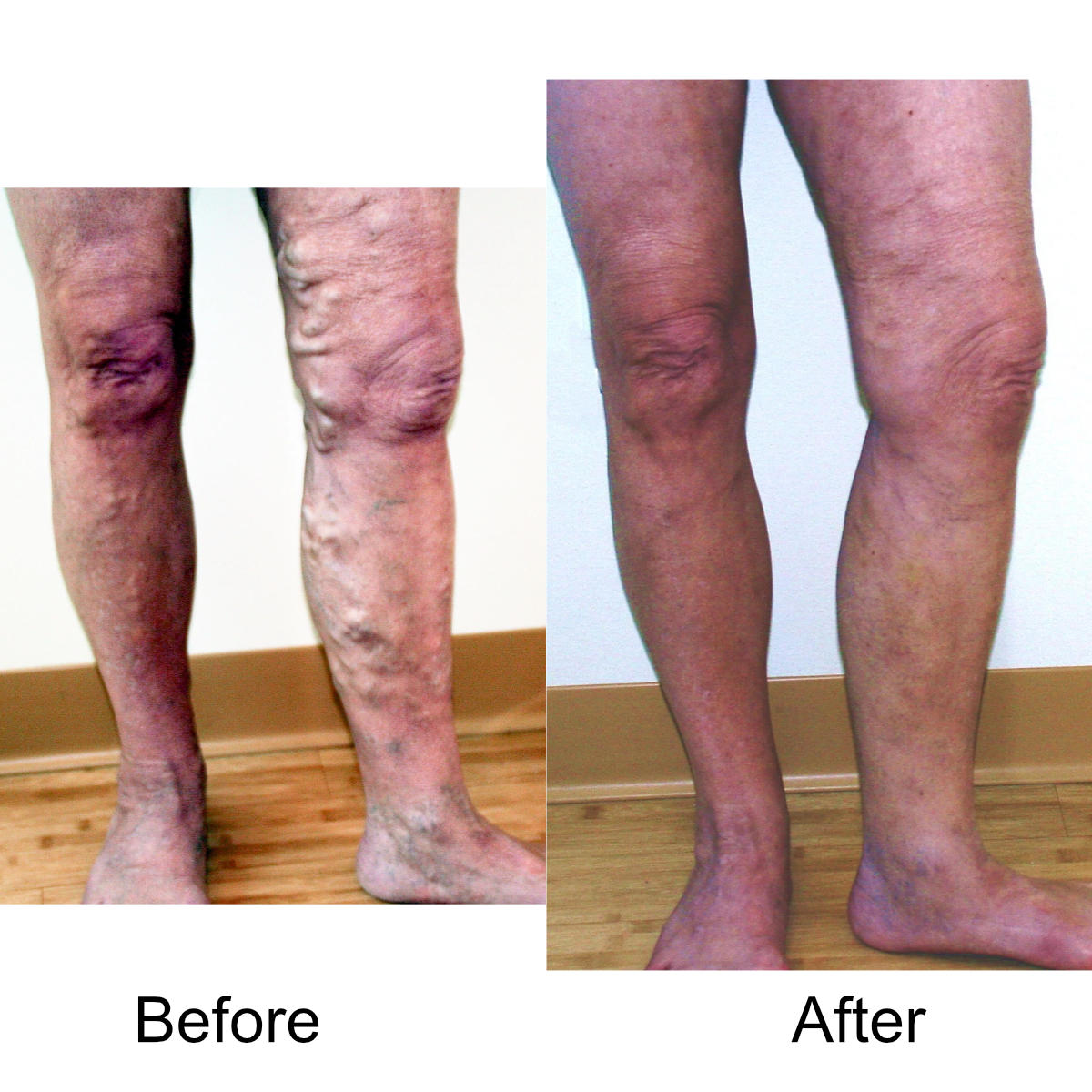
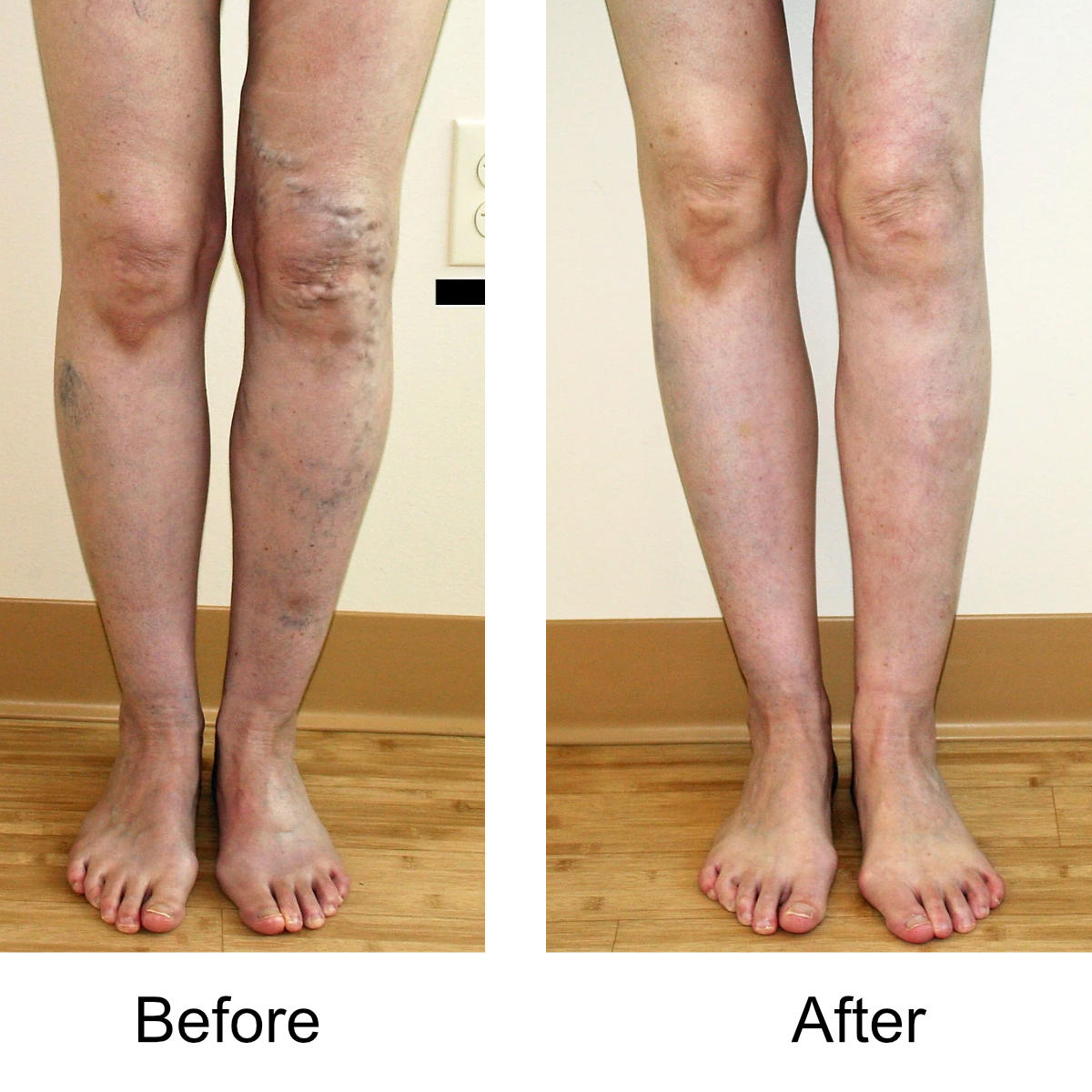
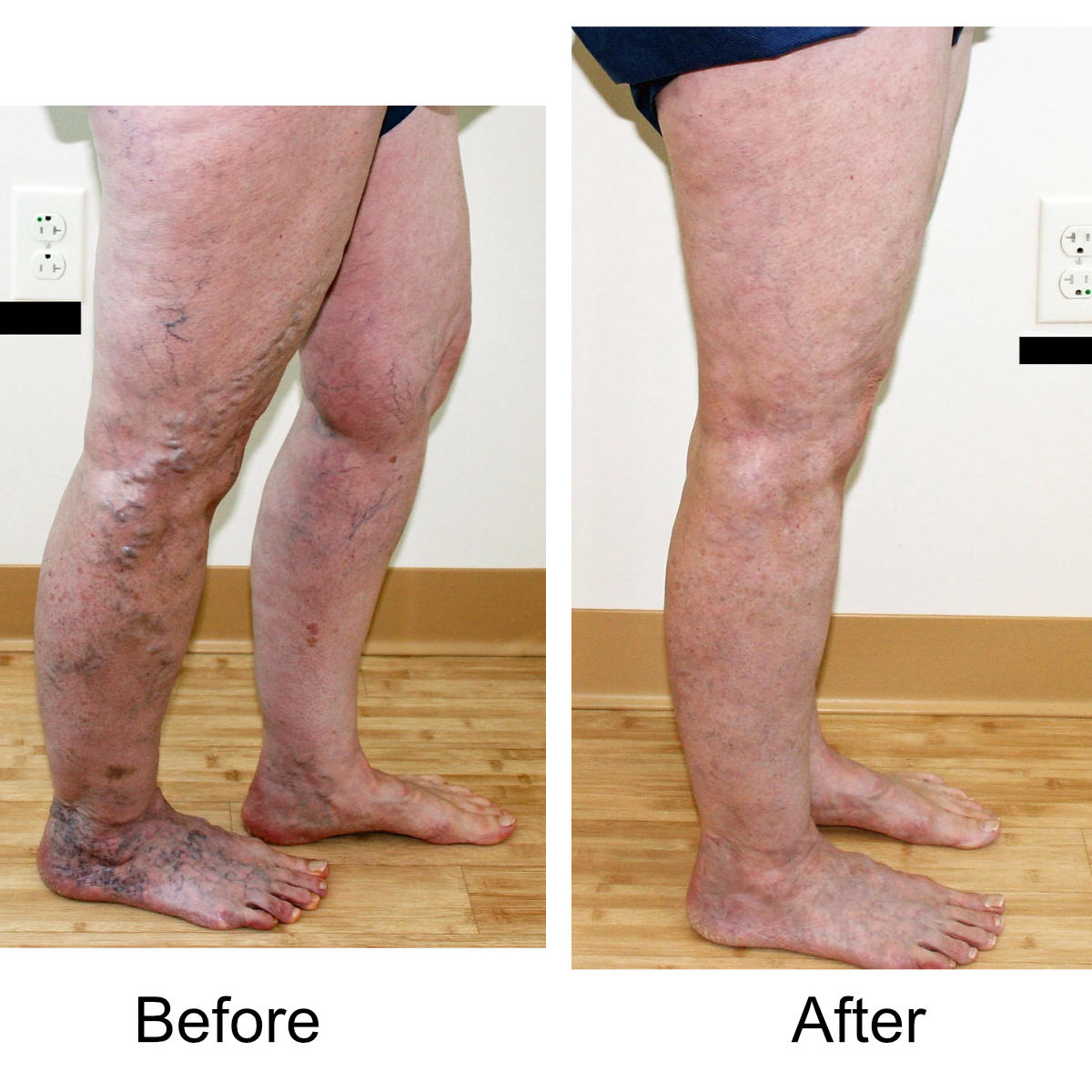
I have massive, ropey clusters of varicose veins all the way down my leg. Will they actually disappear?
Yes. The leg can be significantly disfigured from varicose veins. In nearly all patients, all of the large, bulging veins will vanish and the normal contour of the leg will be restored following treatment.
I love to exercise. Are there any limitations following treatment?
Yes, but only for a short period of time. For small vein treatment, strenuous exertion is not allowed for the rest of the day. For large varicose veins, we usually restrict strenuous exercise for about 1-2 weeks. Fitness can be maintained by walking, which is encouraged during this time.
You say I have large varicose vein disease, but I just want the small veins treated. Why won't you do that?
Large varicose veins are high-pressure veins flowing backwards down the leg. Even if they are not visible from the skin surface, this high-pressure, reverse flow tends to back up into smaller vessels, enlarging them. For the majority of patients with large and small vein disease, proceeding with treatment of the small veins prior to treating the large, underlying vessels will only lead to short-term, unsatisfactory results at best. At worst, it may lead to poor cosmetic results with extensive discoloration of the skin, more veins than you began with, and the waste of a significant amount of your time and money.
I'm planning to have more children. Should I wait to begin treatment?
Pregnancy can cause multiple problems with varicose veins. In most cases, having them treated before your next pregnancy will be to your benefit, and reduce the risk of possible complications during your next pregnancy. Even if additional veins develop with your next pregnancy, they will typically be fewer in number and easily treated following the birth of your child.
Do I have to wear compression hose following treatment?
Compression stockings are needed for 1 week after endovenous thermal ablation, and 2-4 weeks after ultrasound-guided foam sclerotherapy or ambulatory micro-phlebectomy.
Vein Treatment Costs
Questions About Cost
We are often contacted by people who are in need of vein treatment and wish to know what their treatment cost will be prior to being seen by the physician. Unfortunately, there are so many variables related to cost of treatment that it is usually impossible to tell you how much your treatment will cost without actually seeing you first. Variables such as the number of veins that need to be treated, vein size, which procedure or procedures will be best suited to you, number of sessions required for treatment, insurance coverage (including deductibles, policy exclusions, in network vs out of network benefits, etc…) will all make a difference. Therefore, to try to guess the cost breakdown for someone we have not seen is usually impossible.
Pre-Treatment Cost Estimate
That having been said, what we can tell you is that once we have seen you for a consultation, and our office manager has had a chance to review your insurance policy and speak to your insurance representative, we will absolutely be able to give you a cost estimate for your treatment. Furthermore, all out of pocket costs will be established prior to starting any treatment at our office so there will never be financial surprises.
In-Network vs. Out-of-Network Benefits
Finally, several of our patients have requested that we post some information about in-network vs. out-of-network treatment. While many patients will try to have at least some of their work done by an in-network physician, it is always best if that physician is a vein specialist, or at least someone who devotes a significant amount of time to vein practice. The trap here is that some people think they will always save money by seeing an in-network doctor for some of their required treatment. Unfortunately, in many cases this turns out to be false. We have seen patients sent for unnecessary tests, placed under general anesthesia for treatment (never needed!!!), kept in the hospital overnight, and so on, all of which adds up, even if you are only paying an in-network deductible. Those patients end up coming back to us to “complete” their treatment, only to discover that some or all of the treatment needs to be repeated because it was not done properly the first time. When the final costs are calculated it becomes clear that it would have been less expensive to have us take care of the entire treatment from the start.
Still Have Questions? Fill Out the Form Below!
Contact Us

Contact us now to receive more information or schedule a consultation: